Last winter, our local hospital ICU reached capacity during a particularly bad flu season. Three of my coworkers ended up hospitalized with pneumonia. The pharmacist at our neighborhood drugstore said she’d never seen such demand for cough medicine and fever reducers.
That’s when I realized viral pneumonia isn’t just individual health problem – it’s a community issue during outbreak seasons. The way people treat their cases affects hospital capacity, community spread, and overall outbreak severity.
I caught pneumonia that same winter despite my flu shot. Understanding why proper treatment matters beyond just my own recovery changed how seriously I took every aspect of managing the illness.
Reducing Hospital Burden
Hospitals face crisis-level overcrowding during bad flu seasons. ERs overflow, ICU beds fill completely, and healthcare workers burn out from unsustainable patient loads.
Every person who manages viral pneumonia successfully at home is one fewer hospital admission. That freed-up capacity helps the people who genuinely need hospital-level care.
I monitored my symptoms carefully at home – oxygen levels, breathing rate, fever patterns. As long as my oxygen stayed above 92% and fever responded to medication, I could safely recover at home.
Knowing when to go to the hospital versus when to stay home matters enormously during outbreaks. I had clear criteria from my doctor about what symptoms meant I needed emergency care versus what was normal pneumonia progression.
Unnecessary ER visits during outbreaks expose you to additional pathogens and take resources from critically ill patients. I called my doctor’s office with questions instead of rushing to emergency rooms for symptoms that weren’t actually emergencies.
Home pulse oximeters became essential tools during that outbreak season. The $30 device let me monitor oxygen levels objectively instead of guessing whether my breathing difficulty required emergency care.
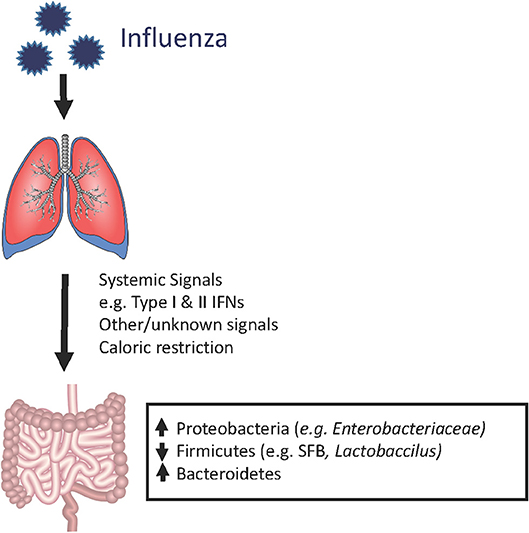
Preventing Community Spread
I isolated completely for three weeks. Nobody visited, I didn’t leave the house, and I wore a mask during the few necessary interactions with family members at home.
This isolation felt extreme, but viral pneumonia is contagious before and during illness. Every person I would’ve infected could’ve developed their own pneumonia, creating exponential spread through the community.
During outbreak seasons, community spread overwhelms healthcare systems quickly. One person infecting three others, who each infect three more, creates unsustainable case numbers within weeks.
I communicated clearly with my workplace about timeline for return. Not “I feel better so I’m coming back” but “my doctor cleared me and I’m no longer contagious.” Returning too early potentially infected coworkers and restarted spread cycles.
Proper treatment speeds recovery, which shortens the contagious period. The faster I recovered fully, the sooner I stopped being a transmission risk to others.
Learning about proper isolation and recovery timelines helped me protect others. Information about treatment and recovery from lung health organizations clarified how long people remain contagious and when it’s safe to resume normal activities.
Antibiotic Stewardship During Outbreaks
During that outbreak, I watched people demand antibiotics for viral infections that don’t respond to antibiotics. Doctors sometimes prescribed them anyway just to satisfy patients, even though they’re useless against viruses.
This unnecessary antibiotic use contributes to resistance – bacteria evolve to survive antibiotics, making the drugs less effective when actually needed. During outbreaks, this becomes community-wide problem.
I trusted my doctor when she explained antibiotics wouldn’t help my viral pneumonia. Testing confirmed viral infection, and antibiotics would’ve provided zero benefit while potentially causing side effects.
Secondary bacterial infections during viral pneumonia DO need antibiotics. But taking them preventatively doesn’t work and contributes to resistance. I monitored for signs of bacterial infection and would’ve taken antibiotics immediately if symptoms indicated secondary infection.
Understanding the difference between viral and bacterial infections helped me avoid demanding inappropriate treatment. This seems minor individually but matters enormously during widespread outbreaks.
Protecting Vulnerable Populations
My neighbor was 78 and immunocompromised from cancer treatment. If I’d infected her with the virus that gave me moderate pneumonia, it could’ve killed her.
During outbreak seasons, protecting vulnerable populations means healthy people treating their illness seriously. My three weeks of isolation protected everyone I would’ve encountered, especially high-risk individuals.
Older adults, people with chronic lung disease, immunocompromised individuals, and very young children all face higher pneumonia mortality rates. Community spread affects them disproportionately.
Getting vaccinated before outbreak seasons provides some protection. I had my flu shot but caught a different strain. The vaccine potentially reduced my symptom severity even though it didn’t prevent illness entirely.
Proper treatment of my case prevented me from being a transmission vector to vulnerable people. That’s part of community responsibility during outbreaks, not just individual health management.
Economic Impact Of Proper Treatment
Three weeks off work felt financially devastating. But returning too early would’ve prolonged illness and potentially caused complications requiring even more time off.
During outbreak seasons, workforce absence affects entire organizations. My team was already short-staffed with multiple people out sick. Adding more absences from people returning too early and relapsing made everything worse.
Proper treatment that achieves full recovery quickly gets people back to work sooner than half-treatments that extend illness. The short-term pain of complete rest beats the long-term problem of chronic symptoms.
Healthcare costs multiply during outbreaks. Every hospital admission, every complication, every extended illness strains insurance systems and drives up costs for everyone.
Managing illness successfully at home costs maybe $100 in medications and supplies. Hospital admission for pneumonia complications costs $10,000-30,000. The math heavily favors proper home treatment when medically appropriate.
Medication And Supply Shortages
During peak outbreak, pharmacies ran out of fever reducers, cough medicine, and pulse oximeters. I bought supplies early when I first got sick, but people getting ill later couldn’t find what they needed.
Hoarding contributed to shortages, but legitimate need during widespread illness depletes supplies quickly. Using medications appropriately instead of excessively helps supplies last for more people.
I took fever reducers only when fever exceeded 102°F, not automatically every four hours. This conservative use made my medicine last longer and left more available for others.
Home remedies – steam, honey, hydration – reduced my medication needs. These approaches don’t replace medical treatment but they supplement it effectively while reducing demand on limited supplies.
Public Health Surveillance
Reporting my illness to my doctor contributed to public health tracking of outbreak severity. This data helps health departments allocate resources and warn communities about outbreak progression.
During outbreaks, real-time illness tracking guides public health responses. School closures, event cancellations, hospital surge preparations – all depend on accurate case numbers.
I participated in voluntary illness reporting through my local health department. Takes five minutes to enter symptoms and testing results, but aggregated data from thousands of people provides crucial outbreak intelligence.
Following treatment guidance from public health authorities helps standardize care and outcomes. When everyone follows similar protocols, health systems can predict and manage resource needs more effectively.
Wrapping This Up
Treating viral pneumonia properly during outbreak seasons matters beyond individual recovery. Hospital capacity, community spread, vulnerable population protection, and economic impacts all connect to how seriously people take treatment.
Proper isolation prevents exponential community spread. Appropriate antibiotic use preserves effectiveness for when truly needed. Complete rest achieves faster recovery and shorter contagious periods.
During outbreaks, individual health decisions become community health issues. Your choice to rest properly or push through illness affects hospital systems, workplace function, and vulnerable neighbors.
Follow medical guidance, isolate completely during contagious periods, monitor symptoms carefully, and use healthcare resources appropriately. These individual actions collectively determine whether communities manage outbreaks successfully or become overwhelmed.